
Rabies
Rabies (lyssa) is one of the oldest known zoonotic diseases, meaning that the disease can be transferred from animals to humans. Humans and animals can get rabies through the saliva of infected animals, when bitten, scratched or licked.
The disease is caused by different lyssaviruses (Lyssa is the Greek goddess of madness). These are viruses that can occur in all mammals. The best known is the classic rabies virus. It occurs worldwide in dogs, cats, ferrets, foxes, and other mammals. It is also present in bats on the American continents and some islands in the Caribbean.
The virus is lethal when treatment is not started immediately. Human-to-human transmission of the infection does not occur. Animals that are infected can pass the virus on before they exhibit symptoms themselves.
Spread
Virus
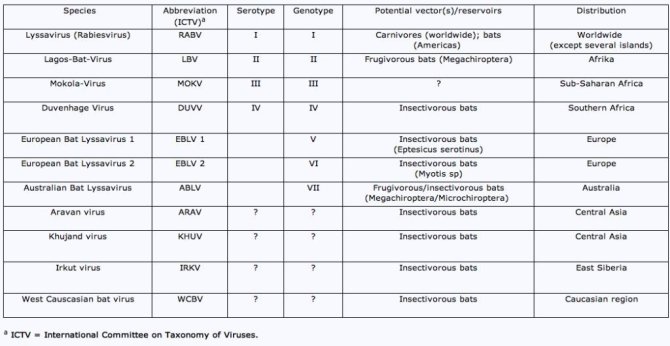
The rabies virus (see figure 1) is a negative-sense single-stranded RNA virus with a distinct bullet shape, which belongs to the order Mononegavirales, family Rhabdoviridae (rhabdo=bullet), genus lyssavirus. Of the lyssavirus genus, 16 genotypes are currently known (table 1). Only genotype 2 has never been found in humans.
Which animals can get infected with rabies in the Netherlands?
The Netherlands is free of the classic rabies virus. In 1987, two related lyssaviruses were found in bats in the Netherlands for the first time. They are both called the European Bat Lyssavirus (EBLV), which is differentiated into two types, namely type 1 (EBLV-1) and type 2 (EBLV-2). EBLV-1 is found regularly in serotine bats (Eptesicus serotinus) in the Netherlands and other European countries. Research has shown that EBLV-1 is present on average in 22% of the sick, weak, or dead serotine bats found in the Netherlands. It is therefore easy for people and pets, usually cats, to come into contact with these animals. We assume this percentage to be significantly lower in populations with ordinary living conditions. EBLV-2 was found a few times in Netherlands in pond bats (Myotis dasycneme), but in other European countries, this type of virus is especially found in the Daubenton's bat (Myotis daubentonii). Several Natterer’s bats (Myotis nattereri) with the Bokeloh Bat Lyssavirus (BBLV) were discovered in Germany and France. The Lleida Bat Lyssavirus (LBLV) was found in Schreiber's bats (Miniopterus schreibersii), a species that occurs elsewhere in Europe, but not in the Netherlands.
It should always be taken into consideration that any type of bat may be a lyssavirus carrier.
Bat rabies and the risk for people
You can only contract an EBLV infection by direct contact with an infected bat. This requires a bite, scratch, or saliva from the infected bat coming into contact with the eyes, nose, mouth, or an open wound. You cannot contract rabies by being in the same space or building as a bat. Bats in wall cavities do not pose a danger to people.
We do not know which viruses the 17 species of bats in the Netherlands harbour, and whether these are harmful to humans. To increase knowledge, Wageningen University & Research participates in the study zoonoses in the night (in Dutch) (2017-2022).
What are the risk groups in connection with bat rabies?
Incubation period
Symptoms
The symptoms of rabies are, especially in the first (prodromal) phase, quite variable and usually start fairly non-specifically, with a slight fever, general malaise, headache, decreased appetite, sore throat, and nausea. The site of the wound may be itchy and painful, which may be a result of the virus multiplying in the sensory nerves.
During the neurological phase, symptoms emerge such as hyperactivity, stiffness of the neck, convulsions, and signs of paralysis, especially in the wound area. In about half of patients, aerophobia or hydrophobia occurs. Feeling air or seeing liquid triggers spasms of the breathing and swallowing muscles, which are so unpleasant that the patient becomes afraid of water.